It is now recognised that right ventricular pacing may, over time, result in left ventricular dysfunction. Consequently, there has been a concerted effort to minimize right ventricular pacing in patients who may not require it.
This has resulted in a range of proprietary ventricular pacing minimization algorithms, that effectively pace AAI(R), but in the event of failed AV conduction will convert to dual chamber-ventricular pacing. After a set or programmable period, successful scheduled conduction testing will once again allow the pacemaker to pace AAI(R).
These algorithms create bizarre ECG appearances that appear to violate the traditional rules regarding the AV delay and the lower rate limit. Consequently, pacemaker malfunction may be suspected. This is a complex topic, partially covered in “fun with ECGs 22”.
Before we describe these algorithms, we need to review the law of AV conduction as it applies to dual chamber pacing.
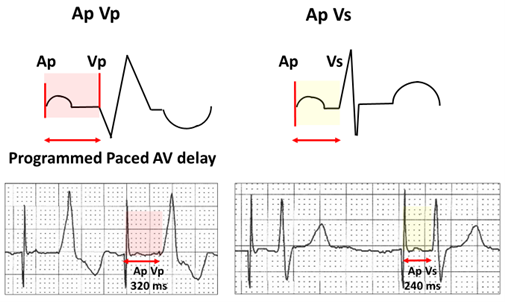
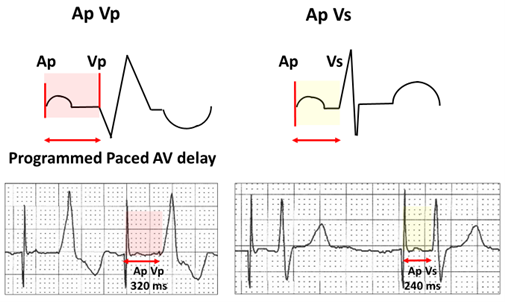
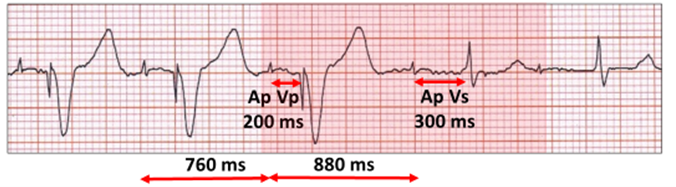
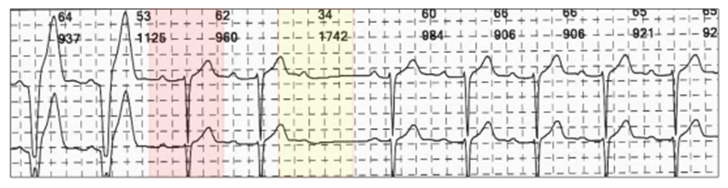
The programmed paced AV delay (Ap Vp, red highlight) is always longer than the sensed AV delay (Ap Vs, yellow highlight). If AV conduction results in ventricular sensing, it is intuitive that it will occur before completion of the AV delay, unless it is a fusion beat.
Ventricular pacing minimization algorithms intentionally violate the law of AV conduction in order to promote ventricular sensing and they can be recognised on the ECG by the ventricular sensed AV delay being longer than with ventricular pacing. There are currently seven unique algorithms from 5 manufacturers, and most can be recognised on the ECG.
These programmable algorithms can be divided into two broad groups, four convert from atrial to dual chamber pacing and three use AV hysteresis in the DDD(R) mode. As the name implies, AV hysteresis allows the AV delay to be extended beyond the programmed value in order to encourage ventricular sensing. The algorithms can be very complex and there are frequent manufacturer software iterations. The details to be given are only those relevant to ECG changes.
On the ECG, there is AAI(R) pacing in patients with intact AV conduction. AV conduction is continually being monitored and a change in pacing from AAI(R) to DDD(R) pacing is referred to as “mode conversion”.
There are two algorithm activation sequences seen on the ECG:
- OFFSET: With failure of AV conduction, dual chamber ventricular sensing changes to ventricular pacing.
- ONSET: Scheduled conduction tests allow restoration of ventricular sensing.
Algorithm-offset: ECG appearance – AAI(R) to DDD(R).
The ECG appearance of algorithm-offset is atrial pacing or sensing followed by failure of AV conduction and dual chamber-ventricular pacing. As the ECG appearances differ for each manufacturer, each will be described separately.
Managed Ventricular Pacing (MVPTM) – Medtronic Inc. Minneapolis MN, USA
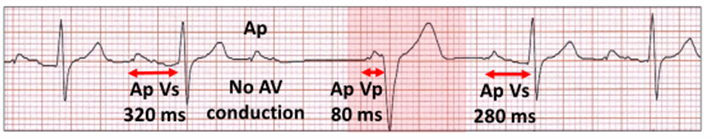
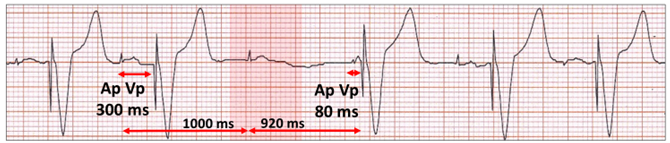
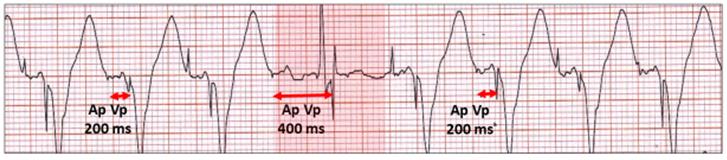
Failure of AV conduction during AAI(R) pacing requires a specific number of events for algorithm-offset and conversion to DDD(R) pacing. If failure of AV conduction occurs for one cycle, then the next atrial paced event is followed by ventricular pacing with a very short 80 ms AV delay.
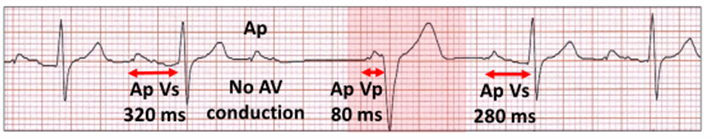
Nocturnal Wenckebach AV block. There is atrial pacing (Ap) with ventricular sensing (Vs) and a dropped atrial paced beat. The next Ap Vp has an 80 ms delay (red highlight). There is mode conversion for one cycle, but no algorithm-offset. The 80 ms AV delay is timed to atrial pacing, so with atrial sensing, the P wave is earlier and thus the AV delay is longer encouraging AV conduction.
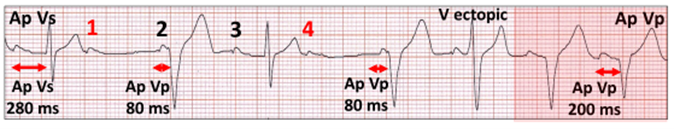
Algorithm-offset to DDD(R) pacing will occur if two of four consecutive cycles have failure of AV conduction. The ECG is diagnostic; atrial pacing/sensing, two failed AV conduction cycles, followed by two short 80 ms AV delays and then AP VP with the programmed AV delay.
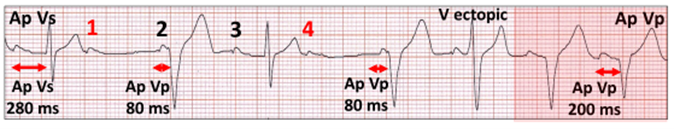
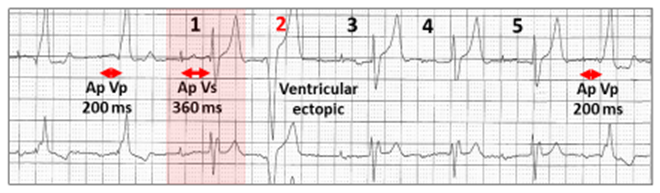
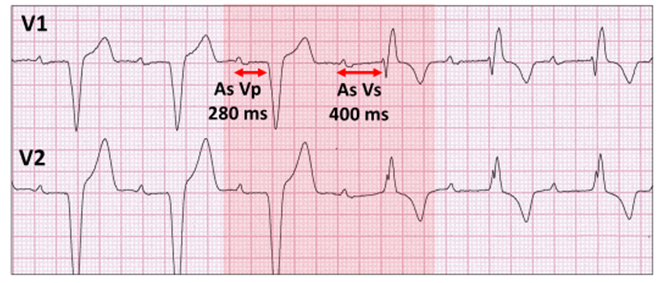
Atrial pacing (Ap Vs) followed by two episodes of failed AV conduction (Ap complexes 1 and 4 in red), both followed by Ap and ventricular pacing (Vp) with an 80 ms AV delay. There is conversion to DDD(R) pacing (red highlight) after a ventricular ectopic. The programmed AV delay of 200 ms is paradoxically shorter than Ap Vs of 280 ms.
SafeRTM – Microport, Clamart, France
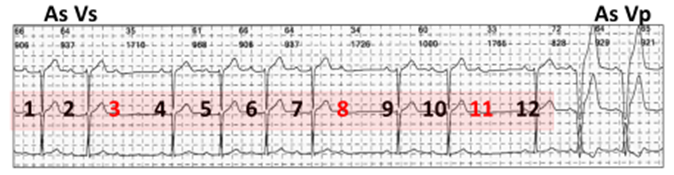
Algorithm-offset requires two consecutive cycles with failure of AV conduction or three in 12 consecutive atrial cycles.
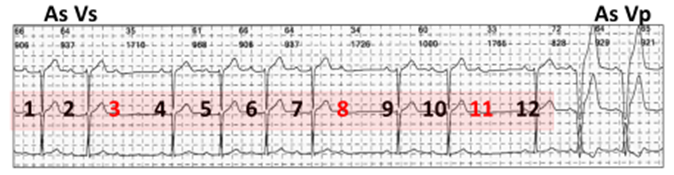
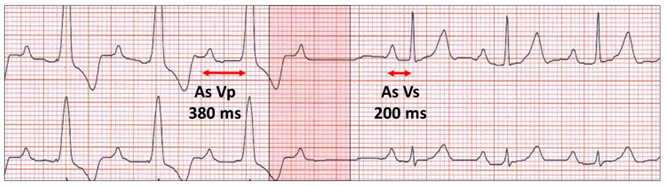
Atrial and ventricular sensing (As Vs). There are three atrial complexes (red) with failure of AV conduction in 12 consecutive cycles (red highlight), resulting in mode conversion to DDD(R) pacing (As Vp).
Vp Suppression – Biotronik, Berlin, Germany.
One of two ventricular minimization algorithms from Biotronik, algorithm-offset will occur after a two second pause or a programmable number of episodes (1 to 4) of failure of AV conduction over 8 consecutive atrial cycles. The appearances would therefore be similar to the above illustration, although the counts can differ.
AV Hysteresis – Biotronik
Being a hysteresis algorithm, failure of AV conduction will result in immediate ventricular pacing with an extended AV delay for five cycles. If there are no sensed intrinsic QRS complexes, the algorithm defaults to the programmed shorter AV delay. There is no linkage of the two Biotronik algorithms and only one can be programmed ON at any one time.
AV Search Plus – Boston Scientific, St Paul, MN, USA
AV hysteresis algorithm with immediate Vp with loss of AV conduction. Two Vp out of 10 consecutive atrial cycles with an extended AV delay will result in algorithm-offset and DDD(R) pacing with a shorter programmed AV delay.
RYTHMIQTM – Boston Scientific
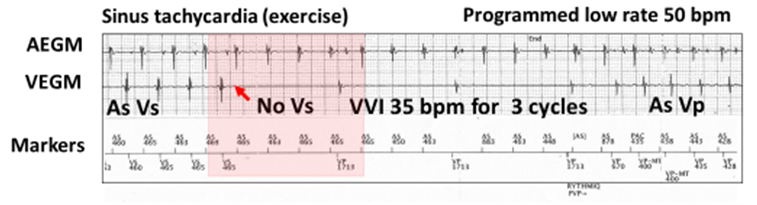
Failure of AV conduction during AAI(R) pacing results in three ventricular paced complexes (VVI) at a rate 15 bpm below the programmed low rate. This can be frightening on the ECG. Telemetered electrograms are helpful.
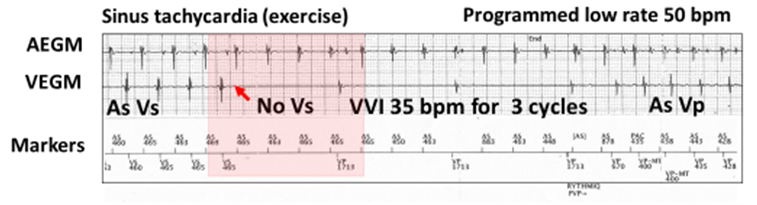
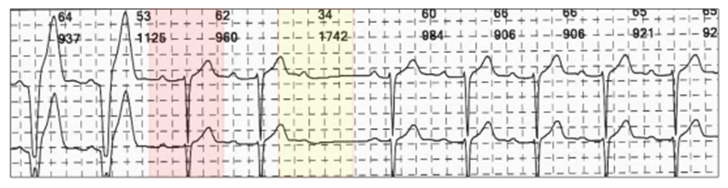
Atrial (AEGM) and ventricular (VEGM) electrograms with markers demonstrating algorithm-offset. The low rate is 50 bpm. During exercise the rate is 125 bpm with atrial and ventricular sensing (AS VS). With AV block and no VS, there is VVI pacing at 35 bpm for three cycles or 15 bpm below the programmed low rate and the patient is pre-syncopal. The slow VVI backup encourages the resumption of AV conduction and intentionally violates the lower rate limit. If no AV conduction, then mode conversion to DDD-ventricular pacing As Vp).
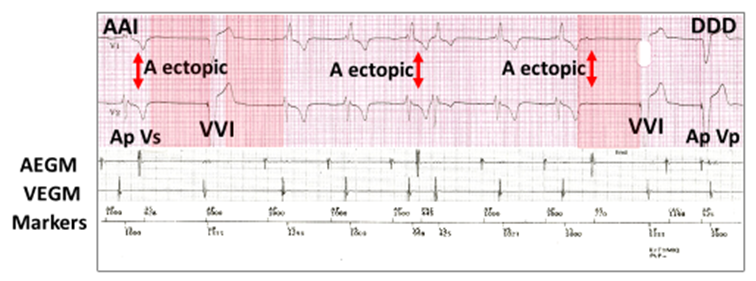
In the more likely scenario of intermittent ventricular escape rhythm, then ventricular sensing will inhibit the full run of VVI pacing, and a complex 3/11 block counter comes into play with a bizarre ECG.
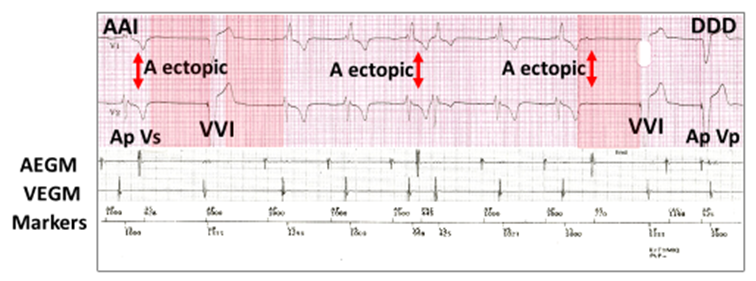
ECG with AEGM, VEGM and markers demonstrating the 3/11 block counter mode conversion from AAI to DDD pacing. The rhythm is AAI with atrial paced (Ap Vs). There are three atrial ectopics (A ectopic, red vertical arrows); the first is concealed and non-conducted, the second concealed, but conducted and the third non-conducted. This results in three pauses out of 11 beats (red highlight); two VVI escape beats (45 bpm) and conversion to DDD-ventricular pacing with the third.
Ventricular Intrinsic Preference (VIP®) – Abbott, Sylmar, CA, USA
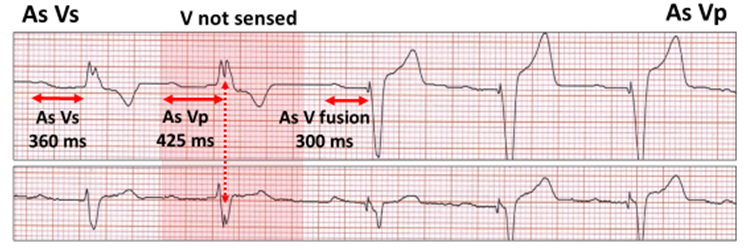
AV hysteresis algorithm. Following failure of AV conduction, there is a programmable extension of the AV window for a programmable one to three cycles.
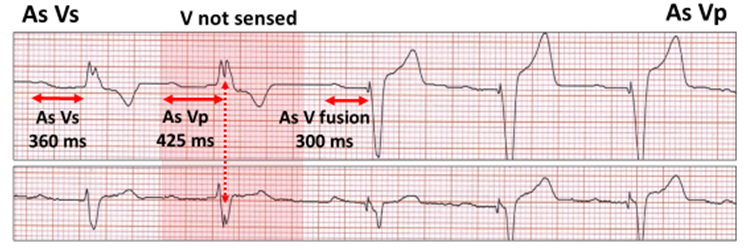
Algorithm-offset after one cycle. There is atrial and ventricular sensing (As Vs). Ventricular under-sensing (red highlight) with a ventricular stimulus artefact (Vp) occurring after an AV delay of of 425 millisecond (ms) for one cycle (red vertical stippled arrow). Ventricular pacing occurs with AV delay shortening to 300 ms initially as fusion.
Algorithm-onset: ECG appearance of DDD(R) to AAI(R).
The ECG appearance of algorithm-onset demonstrates dual chamber-ventricular pacing reverting to ventricular sensing as a result of scheduled conduction tests. These scheduled tests occur with both mode conversion and AV hysteresis algorithms. The timing of the scheduled events may be fixed, programmable and or use artificial intelligence and memory to extend the conducting testing intervals, particularly in the event of continual failed algorithm-onset. Consequently, the scheduled events may occur every few minutes to many hours.
Successful algorithm-onset re-establishes ventricular sensing with a generic ECG sequence.
Successful scheduled conduction (red highlight). Atrial sensing (As) with ventricular pacing (Vp) becomes ventricular sensing (Vs) with apparent violation of the law of AV delay.
There may be a subtle clue as to the manufacturer.
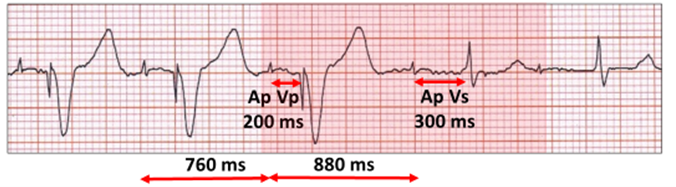
At rest; atrial pacing ventricular pacing (Ap Vp) with an AV delay of 200 ms. During the successful conduction test (red highlight), the AV delay is extended with AV conduction (Vs). The pulse generator is Medtronic because the algorithm extends the Ap cycle length at the commencement of the test for one cycle from 760 ms to 880 ms.
Unsuccessful algorithm-onset with continuity of ventricular pacing may provide unique ECG appearances.
Managed Ventricular Pacing (MVPTM) – Medtronic Inc.
If the conduction test fails, DDD(R) pacing will persist, although the mechanisms for atrial sensing and pacing differ.
In both situations, there will be a dropped P wave and a pause.
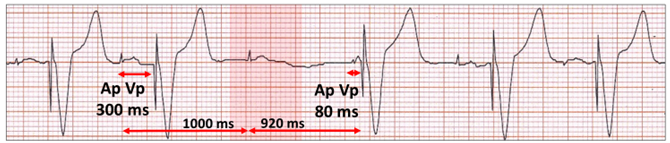
Atrial paced ventricular paced (Ap Vp). With AAI(R) for one cycle (red highlight), there is failed AV conduction followed by ventricular pacing (Ap Vp) with an AV delay of 80 milliseconds (ms). The rhythm continues as Ap Vp.
Atrial sensed ventricular paced (As) Vp. With AAI(R) for one cycle (red highlight), there is a failed conduction test. Remember the timings are based on atrial pacing. The next sensed P wave is therefore earlier and followed by the return of normal AV conduction (As Vs) before atrial pacing (with its 80 ms AV delay). Although it looks like a successful conduction test, the rhythm remains in DDD(R) and further test will follow.
SafeRTM – Microport
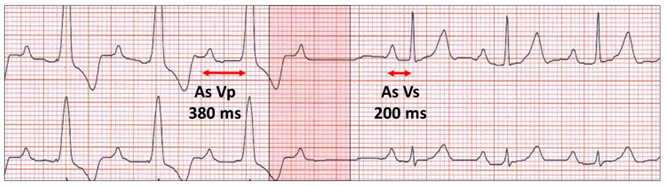
Successful conduction test (red highlight) with mode conversion to AAI(R) pacing.
Two cycles later, however, there is failure of AV conduction, but no mode conversion to DDD(R) pacing as the criteria for algorithm-offset have not been met; two consecutive or three in 12 blocked cycles.
Vp Suppression – Biotronik
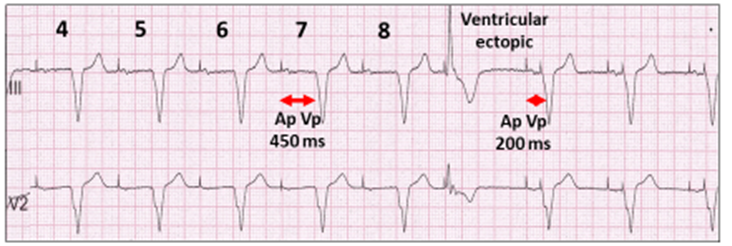
AV extension to 450 ms for up to 8 cycles will occur as part of the scheduled conduction test.
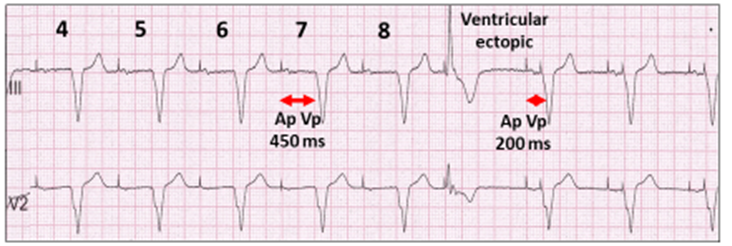
Unsuccessful scheduled conduction test. Atrial and ventricular pacing (Ap Vp) with an extended AV delay of 450 ms for 8 cycles (4 to 8 shown). No ventricular sensing and AV delay shortens to programmed 200 ms with intervening ventricular ectopic.
AV Hysteresis – Biotronik
For successful conversion, there must be ventricular sensing with an AV extension to 400 ms for up to 5 cycles.
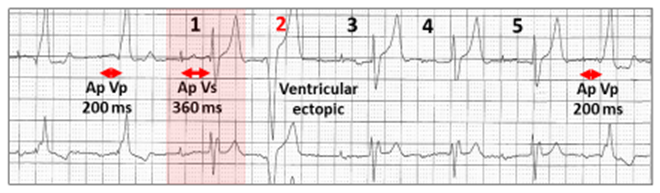
Unsuccessful scheduled conduction test. Atrial and ventricular pacing (Ap Vp). There is an AV extension from 200 ms to 400 ms with ventricular sensing (Vs) at 360 ms (red highlight). There must be Vs for five cycles, but a ventricular ectopic intervenes, which results in a concealed non-conducted Ap, because the ventricle is refractory (red 2). The AV delay shortens to 200 ms.
AV Search Plus – Boston Scientific
There is AV extension for up to 8 cycles.
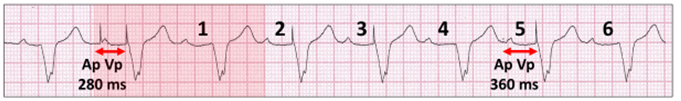
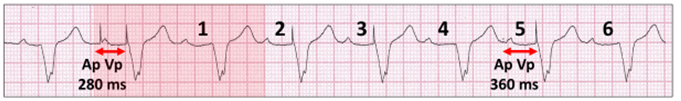
Unsuccessful scheduled conduction test. Atrial and ventricular pacing (Ap Vp).
There is an AV delay extension (red highlight) from 280 milliseconds (ms) to 360 ms for 8 cycles (6 cycles shown) with no AV conduction.
RYTHMIQTM – Boston Scientific
No scheduled conduction tests. To re-establish AAI(R) pacing, AV search plus must be programmed ON as the algorithms work in conjunction for mode conversion.
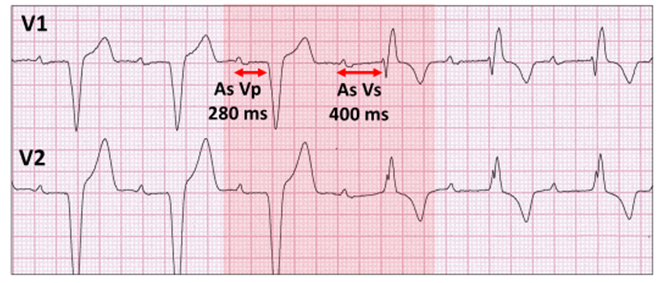
Ventricular Intrinsic Preference (VIP®) – Abbott/St Jude Medical
The AV delay is extended for one to three cycles.
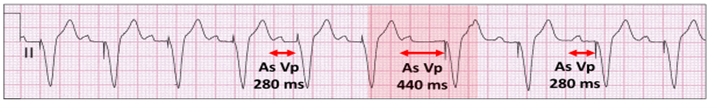
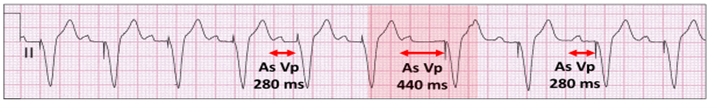
Unsuccessful scheduled conduction test. Atrial sensing ventricular pacing (As Vp) following an AV extension (red highlight) from 280 milliseconds (ms) to 440 ms for 1 cycle. There is no AV conduction.
The scheduled conduction test may be unsuccessful if the conducted QRS is not sensed.
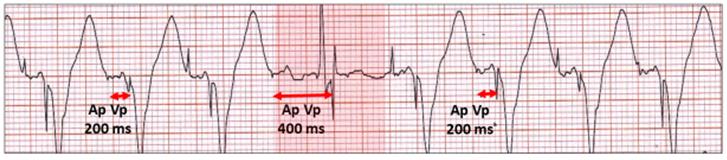
Atrial and ventricular pacing (Ap VP). The AV delay extends from 200 ms to 400 ms for 1 cycle with successful AV conduction, but the intrinsic QRS is not sensed and the ventricular stimulus artefact occurs at 400 ms (highlighted). The AV delay then returns to 200 ms.
It is important to remember that these algorithms can be recognised on the ECG by the apparent violation of the rule of AV delay and when pauses occur, also apparent violation of the lower rate limit.
Harry Mond